Who We Are
Operational Medicine Austere Support (O.M.A.S.) is a 501(c)(3) public benefit charity, that exists to bridge resource gaps in underserved, rural, and austere communities by delivering practical, measurable emergency preparedness and capacity‑building programs that strengthen local readiness, save lives, and keep resources as close to the community as possible.
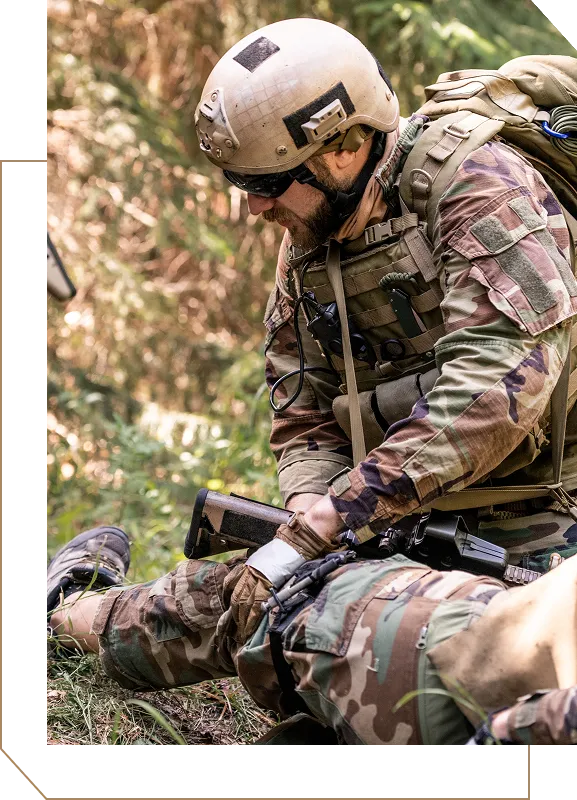
Preparedness
Hands-on hemorrhage control and trauma care training for rural EMS, fire departments, volunteer responders, and community members. No cost to agencies or individuals who can't afford it.
Development
Delivering bleeding control kits, medical supplies, and disaster response gear to agencies with limited budgets.
Support
Medical standby and operational support during wildfires, floods, and community emergencies when agencies are in need of surge resources and personnel.
Community Impact
Where We Serve
Mouse over to interact



















.avif)

.avif)